Synopsis B·Debate – New fronts in the fight against blindness

Nearly 300 million people have serious vision problems, and an estimated one in five people in the world go blind every five seconds. There are many causes of blindness, ranging from such different illnesses as age-related macular degeneration and glaucoma to others that are hereditary, like retinitis pigmentosa and Stargardt disease. Although procedures to slow onset have been developed for some of them, many currently have no effective treatment.
Now, hopes are pinned on multidisciplinary, possibly complementary, studies: more in-depth knowledge of the genes and mechanisms behind blindness, drug cocktails, gene therapy, optogenetics and stem-cell transplants. According to Jordi Monés, director of the Barcelona Macula Foundation, “We are starting down a long, hard road but it will be an exciting trip.”
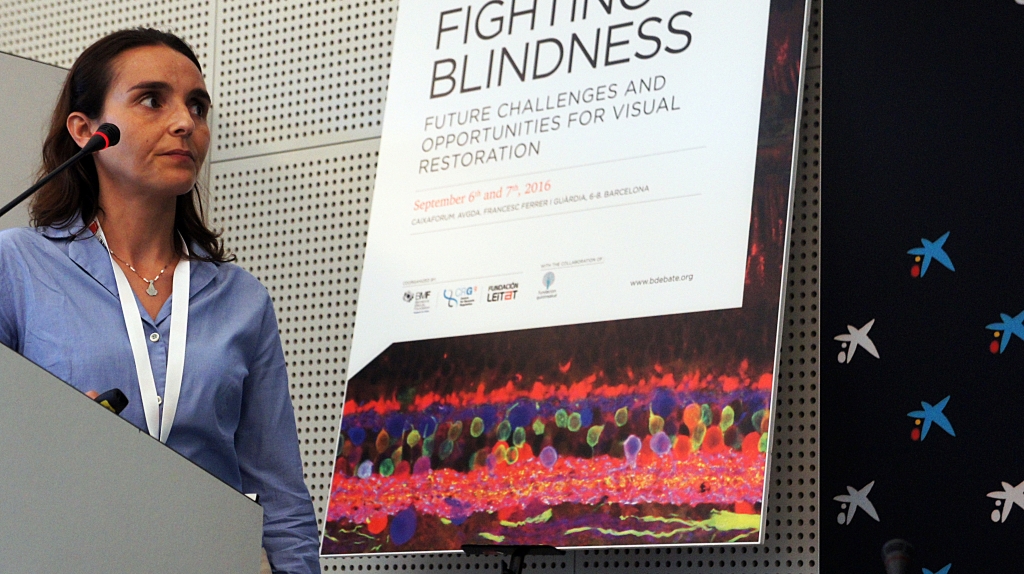
To share and discuss the main news in all of these fields, national and international experts met for a session of B·Debate, an initiative of Biocat and the “la Caixa” Foundation to promote scientific debate. The debate, entitled Fighting Blindness. Future Challenges and Opportunities for Visual Restoration was co-organized by the Barcelona Macula Foundation with collaboration from the Center for Genomic Regulation (CRG) and LEITAT.
Conclusions
- The main cause of blindness in developed countries is Age-related Macular Degeneration (AMD). One of its two forms has no treatment and with the other there can be issues of resistance, which scientists are studying how to overcome.
- The battery of studies includes fields like optogenetics, nanotechnology and visual prosthetics, which so far have only yielded partial results.
- Gene therapy is one of the greatest hopes in fighting visual defects, especially hereditary ones. Scientists are working to make them more effective and safer.
- Regenerative therapy with stem cells is the main hope for very advanced cases. There are currently many studies underway with stem cells to treat different types of blindness. The future will surely be a combination of several therapies.
-
Age-related macular degeneration, a high-priority problem
The macula is a small area of the retina, an approximately one-millimeter yellowish zone, that controls high-acuity vision and allows us to read or recognize faces accurately, for example. For several different reasons, in general mainly due to genetic predisposition along with environmental risk factors like smoking and obesity, age-related macular degeneration (AMD) is the main cause of serious loss of vision in developed countries.
Part of the research being done on AMD is focusing on genetic studies, trying to untangle the causes of the degeneration in order to better attack them. However it is turning out to be particularly complex. According to Marius Ueffing, director of the Institute for Ophthalmic Research in Germany, “We thought that understanding the genome would lead directly to solutions, but it is somewhat more complex and depends on the environment, and can even be random.” In fact, there seem to be very different ways and paths to reach the same result.

Marius Ueffing (Institute for Ophthalmic Research Tübingen).
The studies presented by Caroline Klaver – professor of Epidemiology and the Genetics of Eye Diseases at the Erasmus Medical Center in the Netherlands – show that the genetic variables most frequently associated with AMD have very little influence on risk, and those that do carry more weight are particularly rare among the population. According to Klaver, and paraphrasing psychologist Charles Brewer, “Heredity deals the cards but environment plays the hand.” For example, in order to predict whether a person will develop AMD, we would have to include their age, gender, whether they smoke, their height to weight ratio and up to 26 genetic variables. Even then, up to a third of the high-risk population would not be detected. Plus, Klaver warns, “The tests on the market to calculate this are totally unreliable.”

Caroline Klaver (Erasmus University).
However it’s not all bad news. There are two main types of AMD: atrophic or dry and exudative or wet. For the first, which evolves more slowly, there is no effective treatment. In terms of the second, however, in which new blood vessels form that lead to hemorrhages and bleeding, “There’s been a revolution over the past 15 years,” says Jordi Monés, director of the Barcelona Macula Foundation and scientific leader of this B·Debate session. “It’s as if we had controlled, domesticated Alzheimer”.
One of the first steps was to use laser and photodynamic therapy, which closed up the new blood vessels and contained the hemorrhaging. This allowed doctors to slow the evolution of the disease, to a certain extent, in some cases. However, most patients continued experiencing serious vision loss. The great leap forward came later, with the approval of anti-angiogenic or anti-VEGF drugs, which attack the main growth factor in the pathological blood vessels. These drugs, which are administered in intraocular injections, halt the progress of wet AMD in most patients, even improving visual acuity in some cases.
Research, however, has not stopped. There’s a lot of room to improve in terms of regaining vision, plus over time and with extended treatment some patients develop resistance to drugs or develop fibrosis or atrophy. For these cases, scientists are working on new molecules like anti-PDGF, a growth factor derived from blood platelets that increases visual efficacy and anatomical response, leading to a decrease in fibrosis in the long term. This is the focus of work being done by Samir Patel, cofounder of the Ophthotech corporation, who has launched several clinical trials to test its efficacy.
-
Optogenetics, electricity and nanothecnology to fight blindness
The most novel forms of treatment for blindness can be broken down into two categories. As explained Eduardo Fernández, professor at Miguel Hernández University of Elche, who distinguishes between “biological and technological forms.”

Eduardo Fernández (Universidad Miguel Hernández).
One of the most promising in the first category is called optogenetics and has already begun testing in clinical trials. Studies have started in patients with pigmentary retinitis, an illness that destroys retina cells that capture the light. Optogenetics aims to implant genes from algae into cells that couldn’t capture light, allowing them to do so. This way, ganglion or bipolar cells, which only transmit electrical pulses and are normally spared in many cases of retinal degeneration, become light receptors and take over for the destroyed photoreceptor cells. As Jordi Monés explained, it means a cell “becomes not just a cable but a receptor.”
The therapy, applied in blind patients, does not allow them to recover normal color sight, but doctors do hope they will be able to recognize shapes, read large letters and get around. Meanwhile, as was explained by Marco Zarbin, professor at the Institute of Ophthalmology in New Jersey, scientists are working on new, more sophisticated optogenetic methods to improve results.
The other forms are, to a certain extent, purely technological, using electronic chips. “Vision is based on electric impulses, like an electronic circuit,” says Eduardo Fernández. So, scientists are trying to copy their signals with visual prostheses. They normally have a camera to capture images, a processor to encode them and an electronic circuit board to stimulate the nervous cells, either in the retina or the brain, in the occipital areas responsible for sight. Although some devices have gained approval, it isn’t an easy path: “It’s very difficult to reproduce the patterns of the retina: shapes, colors, contexts, etc.” says Fernández.
One reason for optimism, however, is the fact that the brain is extremely flexible. This was proven in what is considered the first cyborg in the world: Neil Harbisson. This man, who can’t distinguish between colors, has an antenna implanted in his body that transforms them into sounds, allowing him to recognize them using the areas of the brain that control hearing. A study of his brain images revealed the unusual network of connections running to and from this area, which was considerably denser than in a normal brain.
Another important area is nanotechnology, a technological tool that promises to be a vehicle for new biological therapies. According to Víctor Franco Puntes, ICREA professor at the Catalan Institute for Nanoscience and Nanotechnology, nanoparticles offer a wide variety of advantages, including “the fact that they can interact with biology, transport and administer drugs, and even maybe direct implanted cells.” One of the possible applications for blindness lies in using particles that act as antioxidants, but above all it lies in those that can act as a vehicle and facilitate one of the greatest promises in new medicine, along with stem-cell transplants: gene therapy.

Víctor Puntes (Vall d’Hebron Institute of Research, VHIR).
-
The greatest promises: gene therapy and stem cells
Gene therapy
Gene therapy mainly consists in modifying the genetic makeup of the cells to correct a mutation or to give them an advantage to allow them to overcome a defect. It is one of the greatest hopes for many diseases, although for now there is only one type of gene therapy in Europe that has gained approval and it has nothing to do with blindness. It has to do with a type of disease related to the metabolism of fat.
In fact, as explained Francisco J. Díaz Corrales, researcher at the Andalusian Molecular Biology and Regenerative Medicine Center (CABIMER), up to “65% of clinical trials with gene therapy have been done in cancer patients, and only 2% in patients with visual deficits.” However, the eye is a promising organ for this type of therapies. Gema Martínez Navarrete, postdoctoral researcher at Miguel Hernández University of Elche, agreed, “Because it is small, isolated and immunoprivileged” (which lessens the chances of immune rejection of the therapy).
.
Gema Martínez Navarrete (Universidad Miguel Hernández).
One of the problems facing gene therapy is the risks it may imply. Implanting genes into cells is normally done with viruses that go into the nucleus and insert them into the DNA. But it is very difficult to control where they do this, which can lead to undesired mutations. Scientists are working to improve safety and on new formulas like niosomes, a nanotechnology version of the well-known liposomes. And a new repair technology promises to change the future of gene therapy, whether administered by a virus or with nanotechnology. It is called CRISPR/Cas9, and was chosen the most important scientific breakthrough of 2015.
So far, the gene therapy that is the furthest along, which has already been proven to fight blindness, focuses on a hereditary disease called Leber’s congenital amaurosis. Trials are in the pre-approval phase and the therapy has already been tested on 50 patients. According to Díaz Corrales, so far “It has proven safe and effective.” There’s only one mutated gene in this illness, so the design therapy is clear. It would be more difficult in multi-factor pathologies, where there is no specific gene, such as AMD. But it hasn’t been discarded. According to Monés, surely “They are moving towards boosting a protection factor.” Díaz Corrales’ own group is working with this hypothesis on gene SIRT1, a sort of nucleus where several mechanisms involved come together.
Stem-cell transplants
Clinical trials with stem cells to treat various types of blindness began in 2010. And, although no therapies have yet been approved for any sort of visual deficit, “There are currently many clinical trials underway, most with embryonic stem cells,” explained Anna Veiga, director of the Stem Cell Bank at the Center of Regenerative Medicine in Barcelona.

Anna Veiga (Centre de Medicina Regenerativa de Barcelona, CMRB).
Embryonic cells are one of the types that can be used. But there are more: including those called induced pluripotent stem cells (IPS), which are created by reprogramming mature cells to make them into stem cells. These are one of the greatest hopes, although they also have their difficulties. As explained Michael Edel, researcher at the University of Barcelona, these include clarifying issues like “the possibility that they will become tumor cells, knowing whether they provoke an immune response and standardizing and optimizing production protocols.” This isn’t a trivial issue: a trial with the sort of cells to treat macular degeneration had to be halted due to safety issues, as some of the cells had mutations in genes that could cause cancer (oncogenes).

Michael Edel (Universitat de Barcelona).
These cells would be used to replace the damaged ones, as they can mature and substitute those that no longer work to restore lost functions. This is why it’s is called replacement therapy. But there are other options: mesenchymal cells, which come from bone marrow, can also be used. These cells could be used in the earliest stages, as they have protective and stimulating properties that would slow the development of the disease.
And there are even more futuristic therapies being studied. These include reprogramming cells directly in vivo. This is what they are working on in the laboratory of Pia Cosma, ICREA professor at the Center for Genomic Regulation in Barcelona. To do so, they inject ‘activated’ stem cells that go to the retina of rats with pigmentary retinitis and merge with damaged cells. This creates cells that, initially, have two nuclei and seem to regenerate the injured photoreceptors, restoring part of their vision.

Pia Cosma (Centre for Genomic Regulation, CRG).
As Jordi Monés said, «It is a long, exciting road that will probably lead to a combination of these experimental therapies. For the moment, though, we have to test and study them separately».