Stargardt’s disease
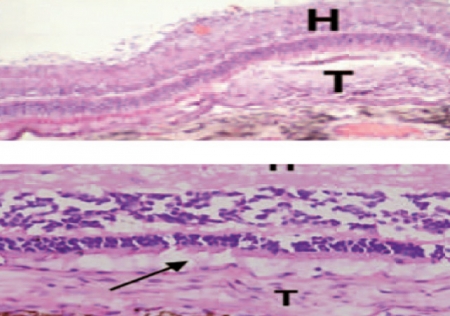
This is the most common macular dystrophy. In the majority of cases it is inherited as an autosomal recessive trait. The vision loss produced by this disease usually affects young people. The incidence of Stargardt’s disease stands at around one person affected in every 10,000, and it usually affects adolescents and young people aged under 20 years. Stargardt’s disease and fundus flavimaculatus are two clinical presentations of the same disease. On a histological level, an accumulation of lipofuscin-type material occurs in the cells of the retinal pigment epithelium due to mutation of the ABCA4 gene. This mutation is inherited when both parents also possess malformation of this gene.
Stargardt’s disease causes blurred vision that lacks sharpness, which hinders the recognition of faces and shapes as well as reading from both close up and from a distance, and in the end it leads to colors of similar shades (for example black and navy blue) being confused with each other.
It also causes difficulty in adapting to shade. Although it does not cause absolute blindness, those affected may lose visual acuity to the point where they reach legal blindness. Patients with this pathology are subdivided into four groups:
- The first, characterized by the beaten bronze color of the ocular fundus and choroidal silence, is the earliest stage of the disease. The back of the eye is almost normal except for the typical “silent” (dark) choroid that shows up in fluorescein angiography.
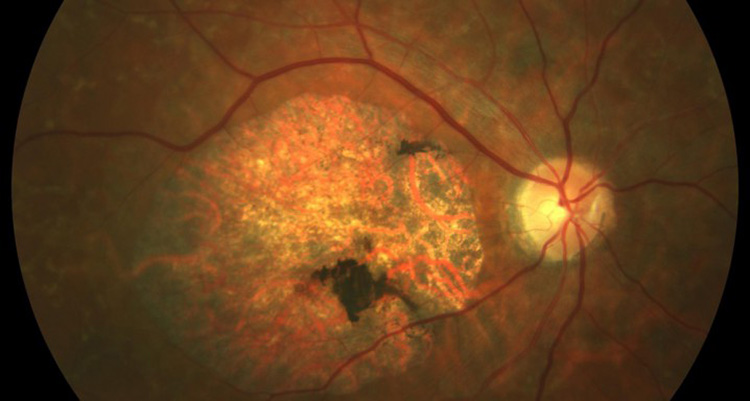
- In the second group, atrophic maculopathy with or without yellow flecks, initially the loss of RPE may be so minimal that in some patients it only shows up when performing the angiogram. Furthermore, the appearance of the bronze fundus and silent choroid may not be evident in the first decade of life. However, later yellowish lesions appear and the storage of lipofuscin becomes evident. The degree and pattern of the zone of atrophy in the macular area vary and do not always correlate with the degree of vision loss. A very common pattern that appears is a doughnut pattern, which in some cases allows visual acuity to be conserved until the age of 40 years. These patients may occasionally develop subretinal neovascular membranes that produce disciform lesions on the macula. The color vision test normally shows slight alteration on the red-green axis. Many patients show prolonged dark adaptation.
- The third group refers to patients with atrophic maculopathy with late signs and symptoms of retinitis pigmentosa. These are similar to those of the second group but at later ages the symptoms and signs of retinitis pigmentosa appear including night blindness and abnormalities of the photopic ERG (in bright conditions and entailing cone dysfunctions) and the scotopic ERG (in dark conditions and entailing rod dysfunctions). Currently it is considered that these patients really suffer a dystrophy of cones and rods produced by severe mutations in ABCA4.
- The fourth group of patients affected by the disease present yellowish flecks not associated with macular atrophy. It is the set of clinical symptoms described as fundus flavimaculatus. These patients may have central and paracentral yellowish lesions associated with minimum angiographic or fundoscopic evidence of atrophy of the RPE between these lesions. There is usually choroidal silence.
Visual acuity may be normal if the center of the fovea is not affected by one of these lesions, although many patients have a large fleck in the foveola and reduced visual acuity. In the absence of information on the rest of the family and in eyes without very clear evidence of choroidal silence it may be very difficult or impossible to differentiate them from a dystrophy in a pattern simulating “fundus flavimaculatus”.
Dr. Jordi Monés, M.D., Ph.D.
COMB Medical license number: 22.838
BMF Medical Director
Doctor of Medicine and Surgery
Specialist in Ophthalmology
Specialist in Retina, Macula and Vitreorretinal
The information provided on the website complements the relationship between the health professional and his/her patient or visitor but does not replace it. If in doubt, you should ask your referring health professional.
BMF carries out a program of clinical trials for researching new treatments for vision diseases. Contact us! You could be the patient we’re looking for.
I want to take part in the clinical trialsStargardt’s disease featured content
Research is the only solution for the future to fight against blindness
It is only with your help that we can fight against blindness
Collaborate