Dr. Jordi Monés explains the hypothesis on the progression to geographic atrophy at the WOC
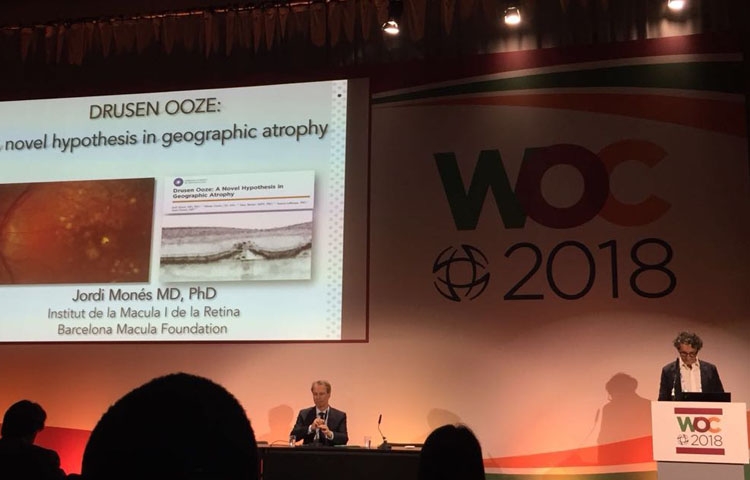
Dr. Jordi Monés, MD, PhD, the Medical Director of the Barcelona Macula Foundation, was invited at the 36th edition of the World Ophthalmology Congress to set out the latest research into macular degeneration, a field in which he is one of the most renowned specialists.
At a meeting that is a benchmark in the ophthalmological world, Dr. Monés presented among other studies the results of “Drusen Ooze: A Novel Hypothesis in Geographic Atrophy”. This describes the new findings on drusen and helps to understand the mechanisms involved in the progression to geographic atrophy. Dr. Monés said that “we are increasingly closer to finding solutions that prevent blindness in patients with AMD”. This work forms part of the European EYE RISK Project, which groups research centres from over six European countries.
Age-related macular degeneration (AMD) is a disease characterised by progressive degenerative lesions to the macula, the part responsible for the finest vision, and it is currently the leading cause of blindness in developed countries. A consequence of AMD progression is Geographic Atrophy, which causes a reduction in visual acuity due to the loss of retinal pigment epithelium and photoreceptors.
The presented study shows that drusen ooze could activate the apical surface of the RPE, exceeding its capacity to maintain the environment of the photoreceptors, which would lead to the death of the RPE, probably through pyroptosis and necroptosis (cellular death mechanisms measured by the inflammation in RPE degeneration in the context of the GA). This would be followed by the continuous, uncontrolled release of intracellular material, which would activate the neighbouring RPE cells even more, would propagate cellular death and would promote the GA progression as a vicious cell-to-cell cycle.
The strength of the study lies in the detailed, precise, dynamic and high-resolution SD-OCT observations of the drusen features and of the progression to GA. These findings may contribute indirectly to increasing our knowledge about the cellular mechanisms involved in GA, and encourage the use of SD-OCT to complement histology to elucidate cellular pathways in retinal diseases.
